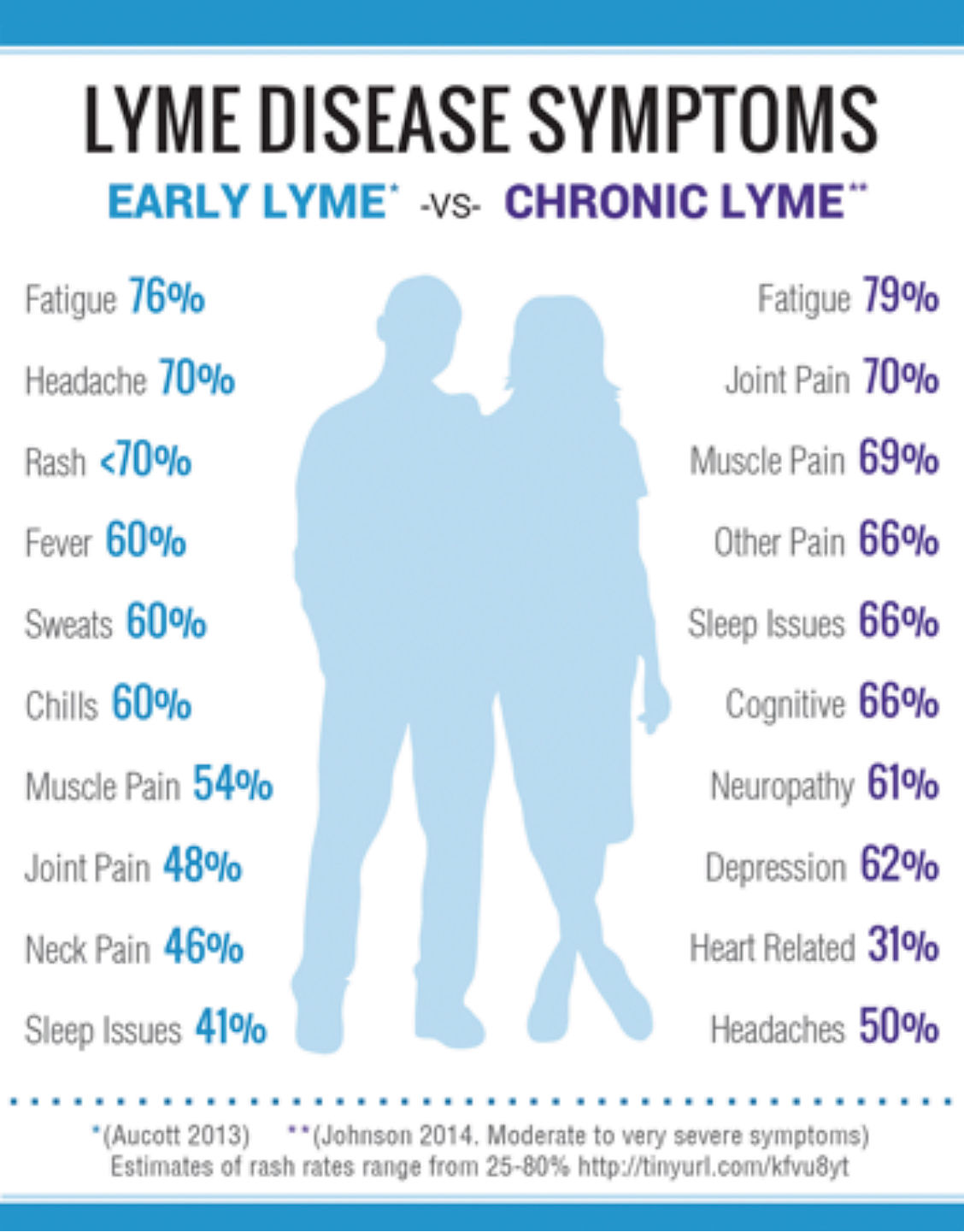
By: Traci Patterson, Founder and Director – Advanced Pathways In August of 2013, the Centers for Disease Control and Prevention announced that cases of Lyme disease are 10 times more prevalent than previously believed, with as many as 300,000 new cases reported each year in the United States. While it remains difficult to diagnose,Continue reading “Lyme Disease and Hypnotherapy”
Tag Archives: #IntegrativeMedicine
How to Handle Cancer Pain: Hypnosis and Self-Hypnosis Pain Relief for Cancer
Cancer pain help through both hypnosis and self-hypnosis may be one of the greatest gifts you give yourself while undergoing treatment for cancer. The pain of cancer can be tremendous but the drugs and other treatments have their own side effects and mind numbing issues that aren’t always desirable. Hypnosis and Self-Hypnosis for Cancer? HypnosisContinue reading “How to Handle Cancer Pain: Hypnosis and Self-Hypnosis Pain Relief for Cancer”
HCT For The Relief and Control Of Chronic Pain
Author: Traci Patterson – Founder and Executive Director, Advanced Pathways You are not your pain. You can make that statement a reality by utilizing the powerful protocol of Hypnosis Combined Therapy (HCT). HCT can harness your ability to retrain neural pathways and develop new patterns in the brain and body, to help you reclaim control.Continue reading “HCT For The Relief and Control Of Chronic Pain”
Researchers Examine Self-Hypnosis to Manage Pain during Needle Biopsy
Author: Beth W. Orenstein Date Published: Jan 29, 2007 Publisher: Radiology Today More than 60% of women in the United States aged 40 and older will undergo mammography screening for breast cancer this year. Between 5% and 10% of their mammograms will result in abnormal or inconclusive findings that will require furtherContinue reading “Researchers Examine Self-Hypnosis to Manage Pain during Needle Biopsy”
CRPS – You Don’t Have To Give In To Your Pain…
I attended the RSDSA conference in LaJolla yesterday. The theme of the conference was, “Treating the Whole Person: Optimizing Wellness.” I love the philosophy behind treating the whole person and optimizing wellness, because that is how each person will regain their life. That’s how I did it! It was a great experience to meetContinue reading “CRPS – You Don’t Have To Give In To Your Pain…”
Outcomes With Hypnosis Combined Therapy by Traci Patterson
Hypnosis Combined Therapy (HCT) by Traci Patterson, CH, CI has proven to be an excellent drug-free, non-invasive, and evidence based treatment protocol that is providing positive outcomes for the patients diagnosed with chronic pain, fibromyalgia, neuropathic pain, chronic migraines, and Complex Regional Pain Syndrome (CRPS) [type 1 and type 2]. Yet it is not limited to theseContinue reading “Outcomes With Hypnosis Combined Therapy by Traci Patterson”
CRPS: Diagnosis and Prognosis
By: Traci Patterson, CH, CI and Owner, Advanced Pathways Hypnosis As an individual that was diagnosed with CRPS (Complex Regional Pain Syndrome) I know there are a lot of questions about how patients are diagnosed and from there what is the prognosis for those patients. I’ve put together some information to try to answer someContinue reading “CRPS: Diagnosis and Prognosis”
Life Lessons I Learned From Cancer
Written by: Traci Patterson, Owner, Advanced Pathways Hypnosis According to the American Cancer Society, the statistics are startling; Cancer is claiming more and more lives every day. The numbers tell us that over 1.6 million people will have been diagnosed by the end of 2014 – a diagnosis that can rock the foundation of anyone’sContinue reading “Life Lessons I Learned From Cancer”